HOME | ABOUT US | MEDIA KIT | CONTACT US | INQUIRE
HOME | ABOUT US | MEDIA KIT | CONTACT US | INQUIRE
You finish college and get that first job as a ball of fire, pulling the late-night shifts, logging the weekend hours at the office and sacrificing family time to help you get ahead. By the time you’re 40, much of that has paid off with a big corner office and the impressive title.
Congratulations. You are now part of a demographic in which:
• More than one person in four, 25.8 percent, has been diagnosed with type 2 diabetes or heart disease.
• More than three in five others, 61.1 percent, are at risk for either of those maladies.
• Nearly half, 45.8 percent, have either high blood pressure, high cholesterol or high glucose levels.
• Almost six in 10 (58.6 percent) are either overweight or obese.
Those stats come from a study by the American Diabetes Association. That same survey proved that a graying America isn’t the nation’s only health challenge—so is denial: Among the 81.6 percent considered at risk for those illnesses, four out of five rated their own health as excellent or good, and fewer than half were willing to change their lifestyles to improve their health.
If there is a true crisis in American health care, it’s not from lack of insurance, since only 13 percent of the population remains without coverage. It’s the growth of diabetes cases, particularly the adult-onset variety, or type 2, which stems largely from the related epidemic—surging obesity rates.
For executives, the challenge of diabetes management is twofold: First, of course, it presents a risk to their personal health and ability to remain fully productive with their organizations. More challenging, given the exploding rates for type 2, is managing its impact on the broader work force.
“As far as lifestyle risks, there is certainly the sedentary, which may apply to some executives,” said Mitchell Hamburg, medical director of the Saint Luke’s Diabetes Center. “Travel also is a big disrupter of lifestyle, in the sense that you’re often eating on the run and maybe not eating the best, since there’s not as much control over your food choices.”
The real lifestyle risk in business, he said, is the choice of where deals get done.
“It may not be the case as much now, but an awful lot of business, particularly in sales, is conducted around food and drink,” Hamburg said. “If that’s the case, both you and your client are at risk for weight gain and diabetes. Stress, to some degree, is a factor, and an area often forgotten is sleep—there’s a lot of evidence that a lack of sleep increases the risk of diabetes. That’s actually a hormonal thing. As you sleep less, your body puts out certain hormones that stimulate appetite, increase the desire to eat, and that affects your weight. Individuals who don’t sleep well or sleep fewer hours are more likely to develop obesity and diabetes.”
Addressing those risk factors can make a bottom-line impact, said David Robbins, director of the KU Diabetes Institute at the University of Kansas Hospital.
“The major health problem, at least in the business marketplace, is type 2,” Robbins said, “and as we get older, as much as 30 percent of people in their 60s are affected by it. Couple that with health care costs overall, and they probably go up 8- to 12-fold when you have diabetes. From a business point of view, you like to keep your staff healthy and not get diabetes, because it’s going to rocket up your costs.”
Diet and exercise, then, are the keys to managing the type 2 threat, but another tool largely overlooked is awareness.
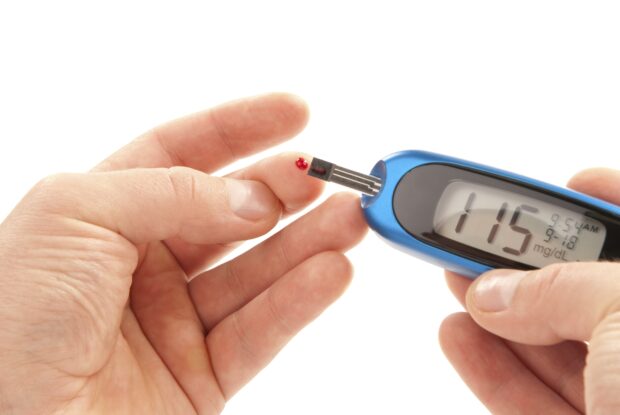
“The other thing that’s important in any workplace wellness program is encouraging individuals to see physicians and get tested to make sure they don’t have diabetes or make sure they’re not at risk,” said Hamburg. “A significant number of pati-ents with diabetes don’t know they have it. At least 10 percent of individuals with type 2 are walking around not realizing that, and if they are not encouraged to see physicians, it may go untreated.”
Lack of aggressive control is one important risk factor, he said. Another: Duration of disease. “The longer you have, more likely you are to have complications develop at any level,” Hamburg said. “Prompt diagnosis can have big benefits over time by improving treatment earlier on.”
Because obesity is the pathway condition to diabetes and a huge range of other illnesses, particularly cardiovascular diseases, it’s important to fight this battle at the margins, health professionals say. That means integrating small steps into daily practices, until they become habits, rather than something to be checked off of a to-do list.
“The biggest myth is that physical activity has to be a tremendous amount to have an impact here, and that’s just not the case,” said Robbins. “Low-level exercise, getting up and around every hour, taking the stairs instead of the elevator, these things
combined, statistically, reduce the risk of getting diabetes.”
Workplace enhancements can also contribute to marginal success, Robbins said.
“There are some clever things being done, but I don’t know if they are being widely adopted yet,” he said. Among them are treadmill/desk combinations that allow for movement while keeping people engaged in their work. “Your productivity increases in some cases,” he said, “as well as keeping you physically active.”
A policy issue contributing to the challenge, Robbins said, is that payments for treatment are based on diagnosis of type 2, rather on pre-diabetic conditions that show themselves at a time where intervention can make a profound difference in controlling the costs of future treatments.
After someone has crossed that personal Rubicon from pre-diabetic to type 2, “over the years that follow, the general course is the need for more and more medication and insulin injections, because the pancreas, those cells die off at an accelerated rate once one has diabetes,” Robbins said. “What we’re learning now is that using certain drugs, starting early in the disease, seems to change that inevitability curve. … The holy grail is preserving the cells that produce insulin, rather than replacing it.”
Robbins’ last point shifts discussions about diabetes control from matters of health-care delivery to issues of research into type 2. Both his program, and research programs at Saint Luke’s, are spearheading lab-based efforts to combat the illness. Those involved in such work say Kansas City is raising its profile for diabetic research, much as it elevated its status in cancer research with the KU Cancer Center’s federal designation as a national cancer center in 2012.
Robbins’ work at KU is complemented by researchers like Mikhail Kosiborod, who is exploring the cardiovascular implications of diabetes through is work at the Saint Luke’s Heart Institute, academic research at the University of Missouri, and at start-up life-sciences companies like Likarda. Co-founded by Lisa Stenho-Bittel, who holds a doctorate in physical therapy, and Karthik Ramachandran, it is now in trials on dogs for a treatment that may regenerate the cells that produce insulin—in effect, producing a cure if that can be translated into human patients.
On all fronts, there is much to be done.
“I think the biggest trend affecting research is the fact that the problem is growing significantly,” Kosiborod said. “If you take the number of patients with diabetes and type 2, it’s really quite alarming.”
Estimates from the Centers for Disease Control, he said, indicate that one in three Americans will have diabetes within a few decades. “That’s likely to have a dramatic impact on diabetes-related complications and costs,” he said. “We need to get a better handle on how to prevent diabetes, and since we know we’re going to see growing numbers, we need to understand better how to treat patients with co-morbidities and different clinical profiles.”
One way his work is contributing to that is through a ground-breaking collaboration to gather data nationwide on patient treatments and outcomes, a big-data project that will produce a national diabetes registry. “It will be a very robust, ambitious national registry of patients with diabetes across the primary- and specialty-care continuum,” Kosiborod said. “We know there’s an epidemic of this, but we have no idea, or very little, of how the quality of care patients are receiving across different practices affects outcomes.”
In Columbia, physician Camila Manrique said her work, too, had exposed her to issues of the cardiovascular implications of type 2, particularly among women.“
Females are more prone to develop cardiovascular disease when they have type 2 diabetes,” she said, “so there is a strong push for developing research data that is translational and significant.” She also said research efforts are moving into explorations of not just the impact of exercise on control, but the timing of that exercise.
“Does exercising before or after a meal have differing impacts on control of glucose or diabetes?” she asked. “And regarding the effect of dietary sugars of liver function, Mizzou has always had a lot of research going on, and that continues to be strong. We’re looking at interventions, lifestyle modifications and exercise.”
The most disturbing trend she’s seeing, Manrique said, is that type 2 diabetes, long considered an adult’s disease, is affecting younger and younger patients, in large part because more children are obese, carrying that weight for additional years through their youth. Perhaps most disconcerting, “we see, unfortunately, people who cannot afford treatment for diabetes.”
Given the increasing importance that controlling diabetes will have in reducing the nation’s issues of health-care costs, it’s an exciting time to be in that line of research, physicians say.
“It is,” Robbins said, “but on the other hand, when I started out in this about 30 years ago, the NIH had what it called a cutoff line where it would fund research. The odds of getting NIH funding then were about 1 in 3; now, it’s 20-1 that you won’t get funded. That has had a chilling effect on young scientists wanting to go into research.”
That’s why much is at stake for this region if it is to elevate is role in diabetes research, physicians say.
“In terms of a national reputation, we’re getting there,” Robbins said. “We’ve reached a point where, as a region, we have momentum. But you have to have the critical mass of institutions to play off one another to get that stamp of approval from the NIH that we are an important center of diabetes research.”